Dialysis and Nutrition - Essential Dietary Guidelines
Nutrition plays a crucial role in the success of dialysis treatment and overall health. When kidneys fail, they can no longer regulate minerals, fluids, and waste products effectively. This makes dietary management essential for preventing complications, maintaining strength, and enhancing quality of life. Working closely with a renal dietitian helps ensure you receive adequate nutrition while avoiding harmful accumulations of certain substances in your blood.
Protein Requirements for dialysis
Dialysis patients need more protein than people with healthy kidneys because some protein is lost during each dialysis session. High-quality protein sources include lean meats, poultry, fish, eggs, and limited amounts of dairy. Aim for 8-10 ounces of high-protein foods daily, distributed across meals. Plant-based proteins like beans and lentils can be included but should be balanced with awareness of their phosphorus and potassium content. Adequate protein helps maintain muscle mass, supports immune function, and promotes healing.
Managing Potassium
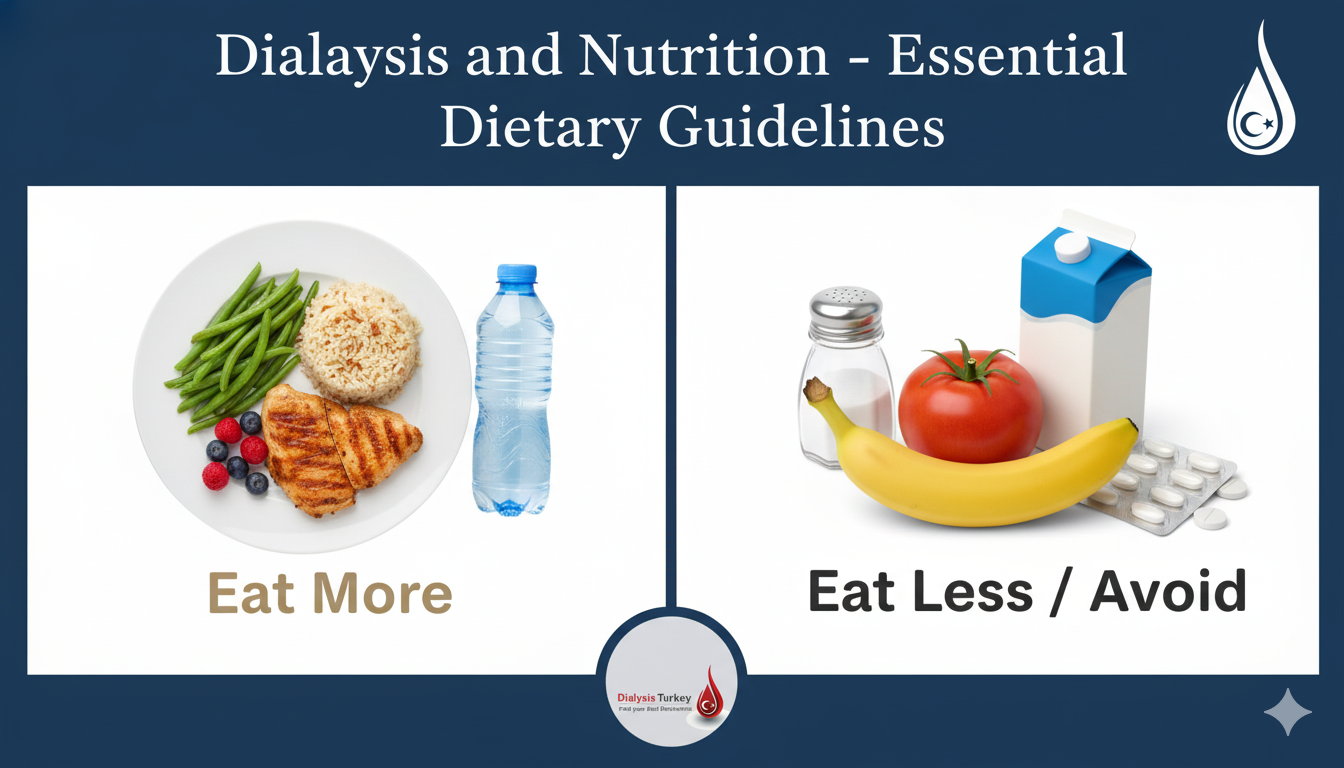
Potassium is a mineral that helps control muscle and heart function. When kidneys fail, potassium can build up to dangerous levels, potentially causing irregular heartbeat or cardiac arrest. Most dialysis patients need to limit potassium to 2000-3000 mg daily. High-potassium foods to limit or avoid include bananas, oranges, potatoes, tomatoes, avocados, and many dried fruits. Lower-potassium alternatives include apples, berries, grapes, cauliflower, green beans, and white bread. Some vegetables can be leached in water to reduce potassium content before cooking.
Controlling Phosphorus
Phosphorus works with calcium to keep bones strong, but excess phosphorus can pull calcium from bones, leading to weakness and fractures. It also causes itching and contributes to cardiovascular problems. Limit phosphorus to 800-1000 mg daily. High-phosphorus foods include dairy products, nuts, beans, whole grains, and dark sodas. You may need phosphate binders, medications taken with meals to prevent phosphorus absorption. Choose lower-phosphorus protein sources like egg whites, chicken, and fish. Reading food labels for phosphorus additives in processed foods is essential.
Sodium and Fluid Management
Controlling sodium intake helps manage blood pressure and reduces thirst, making fluid restrictions easier to follow. Limit sodium to 2000 mg daily by avoiding processed foods, canned goods, restaurant meals, and salty snacks. Use herbs and spices instead of salt for flavoring. Fluid intake is typically limited to 32 ounces daily plus the amount of urine you still produce. Excessive fluid between treatments can cause shortness of breath, high blood pressure, and stress on your heart. Tips for managing thirst include sucking on ice chips, freezing grapes or berries, chewing sugar-free gum, and rinsing your mouth with water without swallowing.
Essential Vitamins and Minerals
Dialysis patients often need supplements because dialysis removes some vitamins and dietary restrictions limit food choices. Your doctor may prescribe B-complex vitamins, folic acid, vitamin C, and vitamin D. Iron supplements or injections may be needed to prevent anemia. Never take over-the-counter supplements without consulting your healthcare team, as some vitamins and minerals can accumulate to toxic levels when kidneys are not functioning properly.
Meal Planning Tips
Successful dietary management involves planning and preparation:
• Work with a renal dietitian to create personalized meal plans
• Keep a food diary to track intake and identify problematic patterns
• Read all food labels carefully, noting phosphorus additives and sodium content
• Prepare meals at home where you can control ingredients
• Find kidney-friendly recipes that appeal to your taste preferences
• Connect with other dialysis patients to share recipe ideas and cooking tips
Remember that diet is medicine for dialysis patients. Following these guidelines helps you feel better, reduces complications, and improves treatment outcomes. Work as a team with your dietitian, adjusting your plan as needed based on lab results and how you feel.